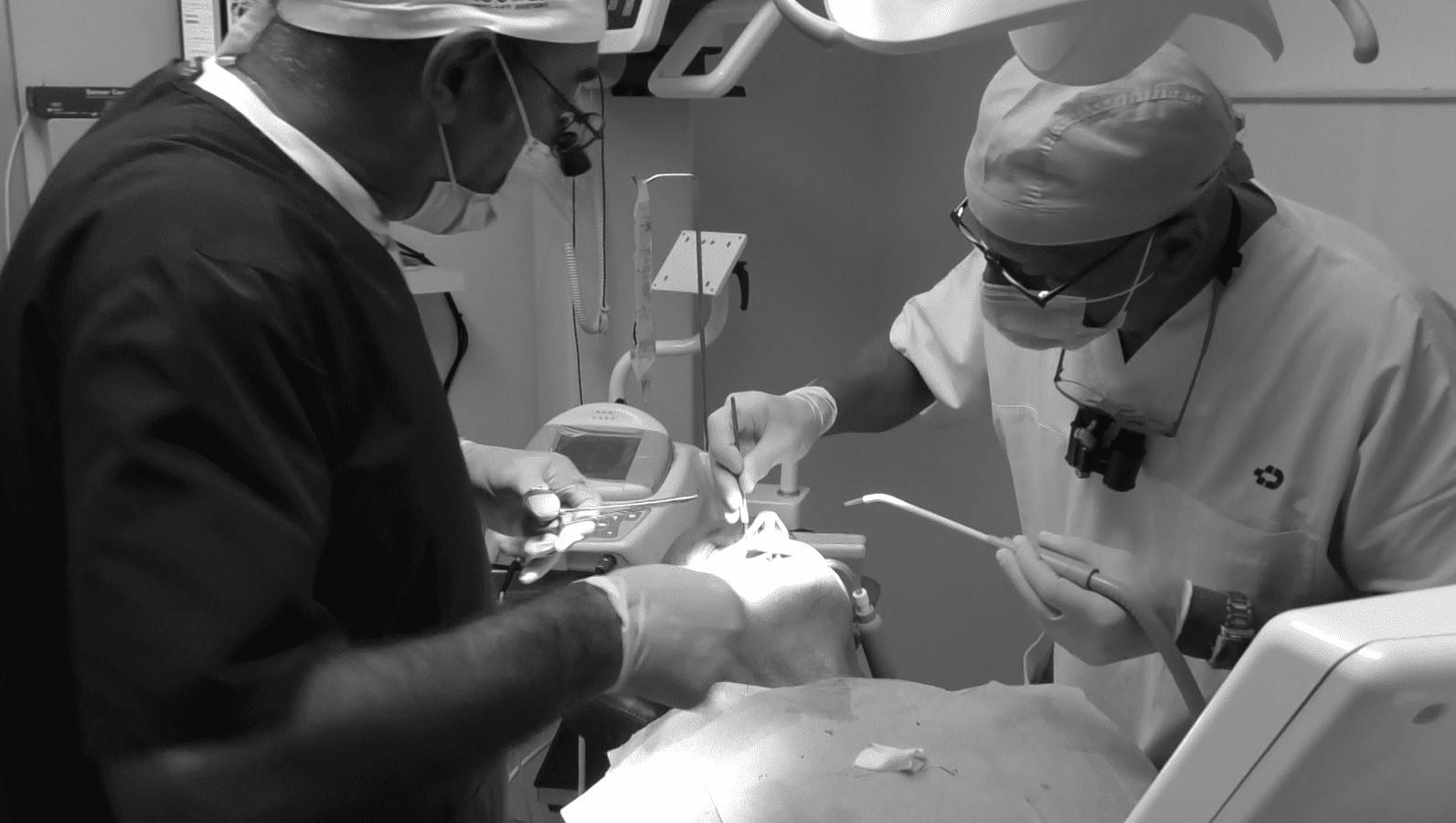
“Explore the Incredible Transformation with Galileus Cerclage Sinus®: Our Revolutionary Surgical Technique in Action!”
Here is a video featuring one of our patients who faced severe challenges due to bone loss in the posterior areas of the upper jaw. Initially, the proposed solutions involved invasive procedures like bone grafts and extensive sinus lifts. However, upon discovering our online center, the patient chose our revolutionary techniques. The outcome? By avoiding traditional grafts, lifts, and prosthetics, he successfully addressed his bone atrophy, achieving a flawless surgical result with a ceramic prosthesis featuring 14 teeth, including molars, ensuring impeccable chewing function and a naturally beautiful smile.
If you’re also seeking a solution for your dental concerns, reach out to us on WhatsApp at +39 3887527525. We’ll respond within 24 hours. Our innovative Galileus Cerclage Sinus® technique will help you regain 100% chewing function, providing an aesthetically pleasing smile. Don’t let bone loss hinder your smile—discover the best solution today.




You have little bone, our solutions without Sinus Lifts and Bone Grafts with Galileus Cerclage Sinus®
Section 1: INTRODUCTION – Research and Challenges in Modern Implantology
In recent times, dental research has focused on maxillary sinus lifts and autologous bone grafts. However, a revolutionary technique, “Galileus Cerclage Sinus®,” often escapes the attention of patients. This series will explore the reasons behind lifts and grafts, highlighting the risks. Finally, we will uncover the “Galileus Cerclage Sinus®,” an innovative solution for patients without bone in the posterior region of the maxillary arch.
Section 2: Why Maxillary Sinus Lifts?
In the first article, we will examine the motivations behind choosing maxillary sinus lifts. We will discuss the conditions that necessitate this procedure, emphasizing the challenges and potential associated risks.
Section 3: The Complex World of Autologous Bone Grafts
The second article will focus on autologous bone grafts, exploring their process, benefits, risks, and disadvantages. We will explain why many people opt for this surgical technique.
Sections 4-6: Details on Autologous Bone Graft and Large Maxillary Lifts
In these sections, we will address separately the autologous bone graft and large maxillary sinus lifts. We will provide details on the procedures, indicating potential complications, and highlighting the challenges associated with each practice.
Section 7: The Risk of Failure in Traditional Procedures
A dedicated article will examine potential failures and complications of traditional procedures, highlighting the uncertainty many patients face with these techniques.
Sections 8-9: The Benefits of Galileus Cerclage Sinus®
In these sections, we present the “Galileus Cerclage Sinus®,” explaining how it surpasses the risks of conventional procedures and offers unparalleled benefits.
Section 10: The Future of Implantology – Choosing the Best Today
We will conclude the series by emphasizing the importance of being informed about available options. We will highlight how choosing the “Galileus Cerclage Sinus®” could represent the future of implant surgery, providing safe, long-lasting, and aesthetically satisfying results.
Conditions Requiring Maxillary Sinus Lifts
- Severe Bone Atrophy:Severe bone atrophy is one of the primary conditions that may necessitate maxillary sinus lifts. In cases where a significant loss of bone volume occurs in the maxillary sinus region, it becomes essential to increase the amount of available bone before proceeding with dental implants. This condition can result from various causes, including:
- Extended Tooth Loss: The lack of stimulation due to tooth loss can lead to significant bone resorption in the maxillary sinus area over time.
- Previous Trauma or Infections: Any traumas or infections in the maxillary region can contribute to bone atrophy, creating a challenge for the stable anchoring of implants.
- Congenital Malformations or Anatomic Anomalies: In some patients, congenital malformations or anatomical anomalies can influence the amount of bone present in the maxillary sinus area.
Maxillary sinus lifts, in these cases, provide the opportunity to create adequate space for the insertion of dental implants, ensuring a solid and stable foundation for future prosthetics. However, it is important to carefully evaluate the risks and benefits of this procedure before making a decision.
Extended Tooth Loss:
Prolonged tooth loss is a key factor contributing to severe bone atrophy in the maxillary sinus. When a tooth is lost and not promptly replaced with a dental implant or another prosthetic solution, there is a lack of stimulation to the maxillary bone. This lack of stimulation initiates a process of bone resorption, wherein the bone gradually loses its density and volume.
The maxillary sinus, located in the upper part of the jaw, is particularly susceptible to this loss of bone volume. Without the structural support provided by teeth, the bone in the sinus area can undergo progressive thinning and weakening. Prolonged bone loss can lead to significant atrophy, posing substantial challenges for the success of dental implants.
Maxillary sinus lifts thus become a crucial procedure to restore the necessary amount of bone to securely support implants. Addressing tooth loss promptly with appropriate interventions can reduce the need for maxillary sinus lifts, underscoring the importance of preventive dental care and timely prosthetic solutions.
Unstable Dentures:
Traditional dental prosthetics can become unstable over time, especially when changes occur in the bone structure of the jaw. The lack of teeth can lead to a narrowing of the bone, influencing the stability of the dentures.
When dentures become unstable, patients may experience functional issues, such as difficulty in chewing and articulating speech. Additionally, the feeling of instability can cause discomfort and self-consciousness in patients, affecting their quality of life.
Maxillary sinus lifts are often considered when dentures become unstable due to bone atrophy. Addressing the situation promptly with appropriate interventions, such as a sinus lift, can contribute to maintaining the stability of dental prosthetics, improving functionality, and enhancing comfort for the patient.
Surgical Complexity:
Maxillary sinus lifts are complex surgical procedures that require considerable precision. The anatomical location of the maxillary sinus adds a significant challenge, as the procedure involves lifting the sinus membrane to create space for bone insertion.
The complexity of the procedure increases when considering the variety of available techniques, including direct or indirect approaches and the use of grafting materials. The choice of technique depends on the specific conditions of the patient, and the surgeon must carefully assess which approach is most suitable.
Furthermore, complexity may escalate in cases requiring additional bone grafts to ensure an adequate amount of bone to support dental implants. Effectively managing these variables demands advanced skills from the surgeon and a customized treatment plan for each patient.
Extended Healing Time:
One critical aspect of maxillary sinus lifts is the extended healing period that patients must undergo after the procedure. Unlike some less invasive procedures, the healing process for maxillary sinus lifts can take several months.
During this period, it is essential for patients to follow the surgeon’s instructions to ensure optimal healing. Restrictions may include limitations in diet, avoiding intense physical activities, and precisely adhering to oral hygiene instructions.
The need for an extended healing time is linked to the nature of the procedure, where the added bone must securely integrate with the surrounding bone before dental implants can be safely placed. Patience and compliance with post-operative instructions are crucial for the long-term success of the treatment.
Potential for Complications:
While maxillary sinus lifts are common procedures, they come with the potential for various complications. It is crucial for patients to be fully informed about these risks before deciding to undergo the intervention.
Among the potential complications is the risk of infections. Since the procedure involves opening the maxillary sinus and adding bone material, there is a possibility of infection during the post-operative period. It is important to carefully follow the surgeon’s instructions to prevent the onset of infections, and if there are any suspicious symptoms, contact the medical professional immediately.
Additionally, the aspect of pain is a significant consideration. After the intervention, patients may experience discomfort and pain. Although the pain is manageable with prescribed medications, it is essential to understand and accept that discomfort may be a temporary part of the healing process.
Finally, adverse reactions to the materials used in the bone graft or implant may occur. It is crucial to discuss any concerns or history of allergic reactions with the surgeon before the intervention to avoid unforeseen complications.
Preventive information is vital to proactively address these potential complications and ensure a better post-operative experience.
Section 3: The Complex World of Autologous Bone Grafts
Autologous bone grafts are a common practice in implantology, often used to address situations of bone atrophy or to enhance the stability of dental implants. However, this complex approach comes with challenges and considerations that patients should understand before choosing this option.
Process of Autologous Bone Graft:
The autologous bone graft involves harvesting bone tissue from the patient, typically from areas such as the hip, tibia, or iliac crest. This tissue is then transplanted into the desired area of the jaw, creating a solid foundation for the placement of dental implants.
Benefits of Autologous Bone Graft:
- Improved Integratability: Being the patient’s own tissue, autologous bone has a higher likelihood of integrating with the surrounding tissue, promoting faster healing and long-term stability.
- Minimization of Rejection Risk: Since the tissue comes from the patient themselves, the risk of adverse reactions or rejection is significantly reduced.
Risks and Challenges of Autologous Bone Graft:
- Pain and Discomfort: Harvesting bone tissue can cause pain and discomfort in the donor area. Careful pain management during the post-operative period is essential.
- Possible Complications: Like any surgical procedure, there are risks of complications, including healing problems, infections, and excessive bleeding.
- Limited Amount of Available Tissue: In some cases, the quantity of available autologous bone tissue might not be sufficient to address extensive atrophies.
- Extended Healing Period: The complete healing and integration of the tissue may take time, prolonging the overall recovery period.
It is crucial for patients to fully understand the risks and benefits of autologous bone grafts before deciding if this is the best choice for their implant needs.
Process of Autologous Bone Graft:
The autologous bone graft process is a surgical procedure involving the extraction of bone tissue directly from the patient and subsequent transplantation into the desired area of the jaw. This approach aims to provide a solid and natural foundation to support dental implants. Here is a detailed overview of the process:
- Preliminary Assessment: Before the intervention, the dentist surgeon conducts a thorough evaluation of the patient. This assessment includes radiographic exams and three-dimensional imaging to determine the amount of available bone and the best location for extraction.
- Anesthesia: Prior to starting the procedure, local or general anesthesia is administered to the donor area (often the hip, tibia, or iliac crest) and the receiving area of the jaw to ensure a pain-free intervention.
- Bone Tissue Harvesting: Using specialized surgical instruments, the surgeon precisely extracts bone tissue from the donor area. This phase requires advanced surgical skills to minimize discomfort and ensure an adequate amount of tissue is collected.
- Preparation of the Receiving Area: Meanwhile, the area in the jaw that will receive the graft is prepared. The surgeon creates small incisions or “pockets” where the bone tissue will be positioned.
- Tissue Transplantation: The harvested bone tissue is then carefully placed in the prepared area of the jaw. The surgeon ensures that the tissue is positioned correctly to ensure proper integration.
- Closure of Incisions: Once the transplantation is completed, the incisions are closed with surgical stitches. This phase is essential to ensure proper healing and prevent infections.
- Post-operative Period: After the intervention, the patient enters the recovery period. It is crucial to follow the surgeon’s post-operative instructions to ensure optimal healing.
Understanding the detailed process of autologous bone grafting is crucial to help patients make informed decisions regarding the management of their implant needs.
Improved Integratability:
A key benefit of autologous bone grafting is its ability to enhance the integratability of dental implants. Bone tissue harvested directly from the patient offers superior biological compatibility compared to synthetic or materials from other sources.
- Biological Compatibility: Autologous bone tissue is a perfect biological match with the patient, reducing the risk of rejection or adverse reactions. This promotes proper integration with the surrounding bone, creating a solid foundation for dental implants.
- Stimulation of Bone Growth: Autologous bone tissue contains vital cells and growth factors that actively stimulate the formation of new bone in the transplanted area. This stimulation fosters a quicker and more complete healing process.
- Minimization of Infection Risk: By using the patient’s own tissue, the risk of infections or complications related to immune reactions is significantly reduced. The autologous nature of the tissue contributes to a safer healing environment.
- Long-term Structural Sustainability: Autologous bone grafting provides a robust and sustainable bone structure over time. Its stable integration into the surrounding tissue helps ensure the long-term durability of dental implants.
- Natural Adaptation: Since autologous bone tissue comes from the same individual, it naturally adapts to the specific anatomical structure of the patient. This adaptation contributes to more harmonious and natural aesthetic outcomes.
Understanding how autologous bone tissue improves the integratability of implants is crucial for those considering this surgical option. The biological compatibility and long-term benefits offered by this technique provide valuable insights in evaluating implant treatment options
Minimization of Rejection Risk:
A crucial aspect of autologous bone grafting is the significant minimization of the risk of rejection. This concept is fundamental when considering procedures involving tissue transplantation, as the body may react negatively to foreign materials.
- Autologous Origin of Tissue: Autologous bone grafting uses bone tissue harvested directly from the same patient undergoing the procedure. This autologous origin drastically reduces the risk of rejection since the tissue is genetically compatible with the patient’s body.
- Avoidance of Adverse Immunological Reactions: The patient’s immune system recognizes its own tissue as “self,” thus avoiding adverse immunological reactions. This prevents rejection that might occur when the immune system attacks and rejects foreign materials.
- Understanding of Own Cells: Cells present in autologous bone tissue are recognized by the patient’s immune system as integral parts of their own body. This familiarity reduces the risk of immune activation and contributes to better acceptance of the transplant.
- Reduced Need for Immunosuppressive Drugs: Unlike transplants involving external donors, the use of autologous tissue reduces the need for immunosuppressive drugs. These drugs are often required to prevent rejection in organ or tissue transplants from different donors.
- Assurance of Genetic Compatibility: Since the tissue comes from the same individual, there is an intrinsic assurance of genetic compatibility. This significantly reduces the risk of adverse events related to genetic differences between the donor and the recipient.
Understanding the minimization of the rejection risk is essential for patients considering autologous bone grafting. This aspect contributes to greater safety and success of the procedure, offering a reliable and well-tolerated option for bone reconstruction.
Risks and Challenges of Autologous Bone Grafting:
While being a widely used procedure, autologous bone grafting comes with some risks and challenges that patients must carefully consider before opting for this technique. It is crucial to fully understand the potentially critical aspects to make informed decisions about one’s dental health.
- Pain and Discomfort: The removal of autologous bone tissue from a donor area can cause pain and discomfort in the harvested tissue area. This may extend the post-operative period and require additional care to manage the discomfort.
- Risk of Infection: Like any surgical procedure, there is a risk of infection associated with autologous bone grafting. It is essential to closely follow post-operative instructions to minimize this risk.
- Possible Complications in the Donor Area: The area from which the tissue is taken may be subject to complications, such as bleeding or healing issues. Although rare events, it is important to be aware of these possible complications.
- Quantitative Limitations of Tissue: The amount of available autologous bone tissue can be limited, especially in patients with significant atrophies. This might require multiple procedures or necessitate consideration of alternatives.
- Prolonged Healing Time: The healing process of autologous bone grafting may take time. It is important to be patient during this period and diligently follow the surgeon’s instructions to ensure optimal healing.
- Possibility of Failure: Although relatively rare, there is a chance of failure of the autologous bone graft. This can be influenced by various factors, including insufficient bone healing or infection in the transplanted area.
- Complexity of the Procedure: Autologous bone grafting is a complex surgical procedure that requires expertise from the surgeon. The complexity of the procedure may increase the risk of errors or complications.
Understanding these risks and challenges is essential to assess the suitability of autologous bone grafting as an option for bone reconstruction. Patients should openly discuss their concerns with their surgeon and carefully weigh potential benefits against risks before making an informed decision.
Pain and Discomfort in Autologous Bone Graft:
Pain and discomfort are significant challenges associated with autologous bone grafts. This surgical process involves removing bone tissue from one area of the patient and transplanting it to another site to stimulate bone growth. Let’s delve into how pain and inconvenience can impact the patient’s experience:
- Pain in the Donor Site: The area from which the autologous bone tissue is taken may experience post-operative pain. This can range from mild to moderate, requiring the use of analgesics to manage discomfort. Pain at the donor site may persist for several days or weeks, contributing to the overall recovery time.
- Discomfort during Healing: The healing phase after an autologous bone graft can be characterized by discomfort. The patient may experience swelling and irritation in the treated area, necessitating special care and precautions to alleviate discomfort. Swelling and irritation can impact the patient’s daily routine.
- Need for Adequate Care: Managing pain and inconvenience requires attention and specific care. Adhering closely to the surgeon’s instructions is crucial to ensure optimal healing and minimize discomfort. This may include the use of prescribed medications, applying ice, and getting adequate rest.
- Individual Variations: The perception of pain and discomfort can vary from person to person. Some patients may experience heightened sensitivity, while others may better manage discomfort. Open communication with the surgeon is essential to tailor the pain management plan to individual needs.
It’s crucial for patients to understand that pain and inconvenience are integral parts of the post-operative process for autologous bone grafts. However, with proper assistance and attention, these factors can be effectively managed, allowing the patient to successfully navigate the healing journey and benefit from the long-term results of the procedure.
Possible Complications:
While autologous bone grafting is a common and well-established procedure, it is essential to understand the potential complications that may arise during or after the intervention. Although rare, these complications require immediate attention and proper management. Let’s examine some of the possible issues:
- Infections: Infections represent one of the potential complications associated with autologous bone grafting. While rare, they can occur during the healing phase. Symptoms of an infection may include swelling and redness in the treated area, accompanied by pain and fever. Timely management with antibiotics is essential to prevent the worsening of the situation.
- Insufficient Graft Healing: In some cases, the transplanted bone may not heal correctly, or poor integration with the surrounding bone may occur. This can affect the stability of the dental implant or the primary goal of the intervention. In such situations, the surgeon may need to evaluate additional strategies to promote healing.
- Persistent Pain: Some patients may experience persistent pain in the graft area even after the expected healing period. This could be caused by various reasons, including nerve irritation or issues with the healing process. The patient should report any persistent pain to the surgeon for a thorough evaluation.
- Adverse Reactions to Anesthesia: Although rare, adverse reactions to the anesthesia used during the bone harvesting procedure can occur. It is crucial to inform the surgeon of any allergies or previous reactions to ensure the use of safe anesthetics.
- Dental Sensitivity: In some cases, autologous bone grafting may influence the sensitivity of surrounding teeth. This is a rare occurrence, but the patient should be aware of the possibility and discuss it with the surgeon before the intervention.
- Abnormal Scarring: The formation of abnormal scars is another potential complication. Scars can become hypertrophic or keloid, affecting the aesthetic appearance of the treated area. The use of appropriate suturing techniques and post-operative care can help minimize this risk.
In general, it is crucial for patients to be informed about the potential risks associated with autologous bone grafting and to work collaboratively with their surgeon to minimize these complications. Open communication and strict adherence to post-operative instructions are crucial for a smooth recovery and positive outcomes.
Limited Availability of Bone Tissue:
Another critical aspect to consider in sinus lifts and autologous bone grafts is the limited availability of bone tissue. The quantity of available bone can be influenced by various factors, including the individual bone structure of the patient, history of tooth loss, and maxillary atresia.
- Individual Bone Structure: Bone morphology varies significantly from person to person. Some patients may have a sufficient amount of natural bone tissue, facilitating the graft harvesting process. In contrast, others may have a thinner or insufficient bone structure, necessitating more complex approaches.
- History of Tooth Loss: Patients with a long history of tooth loss may experience significant bone atrophy in the maxillary sinus area. This phenomenon is common when teeth are lost and not promptly replaced. The lack of bone stimulation can lead to a reduction in bone density, complicating any implant-related interventions.
- Maxillary Atresia: Maxillary atresia occurs when the maxilla does not fully develop or has insufficient dimensions. In these cases, the amount of available bone tissue is naturally limited. Sinus lifts or autologous bone graft interventions can be particularly challenging in the presence of atresia.
The limited availability of bone tissue poses one of the major challenges faced by surgeons during such procedures. It is crucial for patients to understand the specificity of their anatomy and work closely with the surgeon to develop a personalized treatment plan. The individualized approach takes into account the unique characteristics of the patient, helping to maximize the effectiveness of the intervention and minimize associated risks. Open communication between the patient and surgeon is crucial for managing expectations and ensuring optimal results.
Autologous Bone Grafting Process:
Autologous bone grafting is a surgical procedure involving the extraction of bone tissue from the same patient for use in other areas of the body, such as the jaw. Let’s delve deeper into the process of this surgical practice.
- Donor Site Selection: Before the surgery, the surgeon must identify a suitable donor site from which to harvest the bone tissue. Common donor sites include the iliac crest, mandible, or other areas that can provide a sufficient amount of bone.
- Bone Tissue Harvesting: During the surgery, the extraction of bone tissue from the chosen donor site is performed. This can be done through techniques such as aspiration, the use of drills, or other specialized surgical tools. The surgeon works with precision to ensure effective harvesting and minimal discomfort for the patient.
- Preparation of the Receiving Site: After harvesting, the bone tissue is prepared for transplantation. In the case of grafts in the jaw, the receiving site is adequately prepared, often involving the lifting of the maxillary sinus membrane to facilitate the insertion of the bone tissue.
- Attachment of Bone Tissue: The harvested bone tissue is then placed in the receiving site and secured with materials such as screws or other fixation devices. This phase is crucial to ensure the stability of the transplanted tissue and promote the healing process.
- Closure of the Incision: With the bone tissue correctly positioned, the incision is closed with stitches or other suturing methods. Accurate closure of the incision is essential to reduce the risk of infections and facilitate optimal healing.
- Post-operative Monitoring: After the surgery, the patient undergoes a post-operative monitoring period during which the surgeon evaluates the healing and provides any additional instructions for recovery.
Autologous bone grafting is a complex surgical practice that offers advantages in terms of compatibility and reduced risk of rejection. However, its complexity and the prolonged healing period make it a choice that requires careful consideration by patients.
The selection of the donor site is a critical phase in autologous bone grafting, determining the location from which bone tissue will be harvested for transplantation. Surgeons must consider various factors during this phase to ensure the success of the procedure and minimize the impact on the patient. Here are some key aspects of donor site selection:
- Availability of Quality Bone: The donor site must provide a sufficient quantity of high-quality bone. This is essential to ensure that the transplanted tissue has the necessary characteristics to effectively perform its function in the recipient site.
- Anatomical and Functional Compatibility: The donor site should be anatomically and functionally compatible with the recipient site. This means that the harvested tissue should have similar characteristics to those of the site where it will be transplanted, promoting optimal integration.
- Minimization of Patient Discomfort: Surgeons aim to minimize patient discomfort during the donor site selection. This involves choosing donor sites that allow relatively easy access to bone tissue without causing excessive pain or post-operative complications.
- Risk of Complications: Every donor site carries the potential risk of specific complications. For example, harvesting from regions like the iliac crest may be associated with additional risks compared to harvesting from the mandible. Surgeons carefully assess these risks before making a decision.
- Adequate Healing of the Donor Site: After harvesting, the donor site must heal effectively. The ability to restore normal functionality in the donor area is a crucial consideration to ensure the long-term well-being of the patient.
- Adaptability to Surgical Technique: The selection of the donor site must align with the planned surgical technique. For instance, if the surgeon plans to use the harvested tissue for maxillary sinus lifts, they must ensure that the donor site is compatible with this specific procedure.
Accurate donor site selection is fundamental to the overall success of autologous bone grafting. Surgeons, therefore, carefully evaluate all these factors to tailor the approach to the specific needs of each patient.
Bone tissue harvesting is a critical phase in autologous bone grafting, where the surgeon extracts bone tissue from the donor site to transplant it to another part of the body. This procedure requires precision and attention to ensure the success of the intervention. Let’s delve into the process of bone tissue harvesting:
- Local or General Anesthesia: Before commencing with the bone tissue harvesting, the patient undergoes anesthesia to ensure a painless procedure. The choice between local or general anesthesia depends on the complexity of the intervention and the patient’s preferences.
- Incision at the Donor Site: The surgeon makes an incision at the designated body area chosen as the donor site. The selection of the site can vary and may include areas like the iliac crest, the mandible, or other regions based on the specific needs of the intervention.
- Access to Bone Tissue: After the incision, the surgeon gains access to the bone tissue using specialized surgical instruments. Precision is crucial to avoid damage to surrounding tissues.
- Bone Tissue Harvesting: Utilizing tools such as drills or burrs, the surgeon harvests the bone tissue from the donor site. The amount of tissue extracted depends on the specific requirements of the ongoing intervention.
- Closure of the Donor Site: Following the bone tissue harvesting, the surgeon proceeds to close the donor site. This may involve suturing the wound or using other closure methods, depending on the characteristics of the site and the procedure.
- Post-Operative Monitoring: After the procedure, the patient is carefully monitored to ensure proper healing of the donor site. The surgeon provides detailed instructions on post-operative care and symptoms to watch for.
Bone tissue harvesting is a crucial step in many surgical procedures, including maxillary sinus lifts and autologous bone grafts. The choice of the donor site and the harvesting technique directly impact the overall success of the intervention and the long-term health of the patient.
After the bone tissue is harvested from the donor site, the next phase involves preparing the recipient site and securing the bone tissue. This process is crucial to ensure effective integration of
- Assessment of the Recipient Site: The surgeon carefully evaluates the site where the bone tissue will be transplanted. This could be the maxillary sinus for a lift or any other area requiring grafting.
- Creation of an Adequate Receiving Site: If necessary, the surgeon prepares the recipient site by creating a suitable space and adapting it to the dimensions of the harvested bone tissue. This may involve creating a pocket or modifying the area to ensure stable insertion.
- Placement of Bone Tissue: The harvested bone tissue is carefully placed in the recipient site. Precision is crucial to ensure proper adherence and effective integration with the surrounding tissue.
- Fixation of Tissue: The surgeon may use fixation techniques, such as screws or other devices, to stabilize the transplanted bone tissue in the recipient site. This ensures that the tissue remains in the desired position during the healing process.
- Closure of the Recipient Site: After placing and securing the bone tissue, the surgeon closes the recipient site through suturing or other closure methods, ensuring proper healing.
- Post-Operative Monitoring: The patient is closely monitored after the procedure to ensure the proper healing of the transplanted bone tissue. The surgeon provides detailed instructions for the post-operative period.
Preparing the recipient site and securing the bone tissue are critical steps to ensure the success of the graft. Proper integration of the transplanted tissue with the surrounding tissue is essential for achieving lasting results and optimal oral health for the patient.
After completing the process of securing the transplanted bone tissue, the surgeon proceeds with the closure of the incision. This is a crucial step in ensuring proper healing and minimizing the risk of infections. Here is how the closure of the incision takes place:
- Precise Alignment: The surgeon carefully aligns the edges of the incision to ensure accurate closure. This is crucial for optimal healing and minimizing undesirable scarring.
- Use of Suturing Materials: High-quality suturing materials are used to close the incision. The choice of suture type depends on the size of the incision, its location, and the surgeon’s preference.
- Suturing Technique: The surgeon employs a suturing technique that promotes uncomplicated healing. This may include single or multiple stitches, depending on the specific requirements of the case.
- Hermetic Closure: The goal is to achieve a hermetic closure of the incision to prevent potential infections and facilitate smooth healing.
- Protection of the Treated Area: After closing the incision, the treated area may be protected with dressings or other appropriate devices to prevent accidental trauma during the post-operative period.
- Post-Operative Instructions: The surgeon provides the patient with detailed instructions for wound care during the healing period. This may include guidance on cleaning the area, medications to take, and any signs of complications to monitor.
Proper closure of the incision is essential for the success of the procedure and to avoid post-operative issues. Meticulous attention to this step contributes to ensuring quick and uncomplicated healing for the patient.
Post-operative monitoring is a crucial phase in the healing process after an autologous bone graft surgery. During this period, the patient and the medical team collaborate to ensure optimal recovery and prevent any complications. Here is how post-operative monitoring is managed:
- First Hours After the Surgery: In the initial hours after the surgery, the patient is closely monitored to ensure a positive response to anesthesia and to check for any signs of excessive bleeding or other immediate issues.
- Guidance for Pain and Inflammation: The patient receives detailed instructions on pain and inflammation control. Analgesic or anti-inflammatory medications are prescribed if necessary, and the patient is instructed on how to take them correctly.
- Instructions for Oral Hygiene: Specific instructions for oral hygiene during the post-operative period are provided to the patient. This may include the use of saline solutions for rinsing or other practices to keep the treated area clean.
- Follow-up Appointments: Follow-up appointments are scheduled to closely monitor the healing process. During these meetings, the surgeon may examine the treated area, remove any stitches, and assess the overall progress of healing.
- Detection of Early Complications: The patient is educated about signs of possible complications, such as infections or abnormal bleeding. If worrisome symptoms occur, it is important to immediately contact the medical team.
- Radiographic Check: In some cases, radiographic checks may be planned to evaluate the proper integration of the transplanted bone. These checks allow the surgeon to confirm that the healing process is progressing as expected.
- Adjustments to the Care Plan: Based on the individual patient’s response, the care plan may be adapted. This could include modifications to pharmacological therapy or the follow-up schedule.
- Psychological Support: The patient may receive psychological support to address any anxieties or concerns related to the surgical intervention and the healing period.
Post-operative monitoring aims to ensure that the patient goes through the healing phase safely and effectively. Open communication between the patient and the medical team is crucial to promptly address any issues and ensure a positive recovery.
Section 5: Large Maxillary Sinus Lifts: Pros and Cons Surgical Complexity:
Large maxillary sinus lifts, also known as maxillary sinus lift procedures, represent a complex surgical approach. This practice involves lifting the maxillary sinus membrane to create space for the insertion of dental implants. The complexity of the procedure can lead to various pros and cons.
Pros:
- Significant Bone Gain: Large maxillary sinus lifts allow for a substantial amount of additional bone. This is particularly advantageous for patients with severe bone atrophy in the posterior maxillary region.
- Adequate Support for Implants: The increased bone volume provides a solid and adequate foundation for the insertion of dental implants. This can enhance the stability and longevity of the dental implants.
Cons:
- Surgical Complexity: The maxillary sinus lift procedure is surgically complex and requires an in-depth understanding of the anatomy of the region. The complexity increases the risk of intra and post-operative complications.
- Prolonged Healing Time: After a large maxillary sinus lift, patients must undergo a prolonged healing period. The need to wait for the new bone tissue to fully integrate can extend the overall treatment timeline.
- Potential Risks: The procedure comes with associated risks such as sinus membrane perforation, infections, and potential procedure failure. These risks need to be carefully evaluated before proceeding with the surgery.
- Anatomic Limitations: Not all patients are suitable candidates for this procedure due to anatomic limitations. A thorough assessment of the bone structure and individual patient characteristics is essential.
In conclusion, large maxillary sinus lifts offer significant benefits in terms of bone recovery but must be balanced with a thorough understanding of associated risks and challenges. The decision to undergo this procedure should be based on a detailed case assessment by the surgeon and open communication with the patient.
Section 6: Risk of Failure in Traditional Procedures
The Risk of Failure in Traditional Procedures
Potential Causes of Failure:
- Postoperative Infections: Traditional procedures increase the risk of postoperative infections, which can compromise the healing and integration of the transplanted bone.
- Insufficient Integrability of Transplanted Bone: Despite careful selection and preparation of the donor site, the transplanted bone may not optimally integrate with the surrounding tissue, leading to intervention failure.
- Complications Related to Autologous Bone Graft: The autologous bone grafting procedure may involve complications such as a limited amount of available tissue, prolonged postoperative pain, and the potential for tissue rejection.
- Issues related to Maxillary Sinus Lift: While effective in providing space for implants, this practice may be subject to risks such as perforation of the sinus membrane, increasing the chances of failure.
Importance of Personalized Assessment:
Each patient is unique, with individual anatomical features and health conditions. A personalized assessment is crucial to identify specific risks that a patient may face during or after the procedure.
Future Perspective with Galileus Cerclage Sinus®:
Introducing Galileus Cerclage Sinus® as a revolutionary alternative to these traditional procedures can mitigate many associated risks. This innovative technique provides a safe solution, minimizing potential failures and ensuring reliable long-term results.
In conclusion, understanding the risk of failure in traditional procedures is essential to guide patients towards safer and more effective treatment choices. The evolution of technology and the introduction of new methodologies like Galileus Cerclage Sinus® pave the way for a safer and more efficient implant future.
Postoperative Infections in Maxillary Sinus Lift and Autologous Bone Grafting Procedures
Postoperative infections represent one of the potential complications of traditional maxillary sinus lift and autologous bone grafting procedures. While these interventions are widely used, they can expose patients to infection risks that require careful management and prevention.
Causes of Postoperative Infections:
-
- Contamination of the Surgical Site: During surgery, the surgical site is vulnerable to the entry of bacteria or other pathogens. Contamination can occur during tissue manipulation or from the surrounding environment.
- Inadequate Wound Management: Postoperative care is crucial to prevent infections. Inadequate wound management, such as improper cleaning or the absence of sterile dressings, can increase the risk of infections.
- Immunosuppression: Some patients may be more susceptible to postoperative infections due to pre-existing medical conditions or immunosuppression. Weakening of the immune system can compromise the body’s ability to fight pathogens.
Prevention of Postoperative Infections:
-
- Sterile Procedures: The use of sterile surgical techniques and controlled environments is crucial to prevent surgical site contamination during the procedure.
- Antibiotic Therapy: In some cases, the doctor may prescribe preventive antibiotic therapies to reduce the risk of infections. However, appropriate antibiotic use is essential to avoid bacterial resistance.
- Postoperative Instructions: Providing detailed instructions to the patient for postoperative care, including wound cleaning and the use of any prescribed medications, is crucial to reduce the risk of infections.
Management of Infections:
In the event of a postoperative infection, timely intervention is crucial. This may include:
-
- Appropriate Antibiotic Therapy: Prescribing antibiotics targeted to combat the specific infection.
- Proper Drainage: In some cases, drainage of any collections of infected fluid may be necessary.
- Continuous Monitoring: Careful monitoring of the patient’s condition and wounds to ensure that the infection is under control.
In conclusion, the management of postoperative infections is an essential part of post-surgical care. Prevention, early identification, and effective management are crucial to ensuring positive outcomes in the healing process.
Insufficient Integrability of Transplanted Bone in Maxillary Sinus Lift and Autologous Bone Grafting Procedures
Insufficient integrability of the transplanted bone is one of the challenges that may arise in traditional maxillary sinus lift and autologous bone grafting procedures. This issue occurs when the transplanted bone tissue does not optimally integrate with the surrounding bone, leading to potential complications and compromising the success of the intervention.
Causes of Insufficient Integrability:
-
- Tissue Ischemia: During the grafting process, blood supply may be compromised, leading to tissue ischemia in the transplanted bone. This can negatively impact the bone’s ability to heal and integrate.
- Micro-Movements: Excessive movements or micro-movements of the transplanted bone can hinder the healing and integrability process. Graft stability is crucial for its success.
- Bacterial Contamination: Infection can compromise the effective integration of the transplanted bone. The presence of bacteria at the surgical site can delay healing and lead to integrability issues.
Complications Related to Insufficient Integrability:
-
- Resorption of Transplanted Bone: If the transplanted bone does not integrate adequately, there is a risk of resorption, where the body absorbs the bone tissue, compromising the graft’s structure.
- Implant Instability: In cases involving dental implant procedures associated with bone grafting, insufficient integrability can cause instability of dental implants.
- Need for Additional Interventions: Insufficient integrability may require additional interventions to address the situation, increasing the complexity of the treatment.
Approaches to Improve Integrability:
-
- Advanced Surgical Techniques: Utilizing advanced surgical techniques, such as Galileus Cerclage Sinus®, can contribute to improving integrability by reducing risks associated with traditional procedures.
- Continuous Monitoring: Postoperative monitoring is essential to detect early signs of healing or integrability issues.
- Proper Management of Complications: In case of issues, timely intervention with targeted procedures and appropriate management is crucial.
- Treatment Personalization: A personalized treatment approach, considering the patient’s specific conditions, can contribute to improving the integrability of the transplanted bone.
In conclusion, insufficient integrability of transplanted bone is a serious challenge that requires attention and careful management. The adoption of innovative approaches can play a key role in enhancing the overall outcomes of maxillary sinus lift and autologous bone grafting procedures.
Complications of Maxillary Sinus Lift: Addressing Associated Risks
Maxillary sinus lift is a complex procedure that may entail various complications. Let’s examine some issues related to this practice:
-
- Perforation of the Sinus Membrane: During maxillary sinus lift, there is a risk of perforating the sinus membrane, leading to complications such as sinus infections and jeopardizing the success of the intervention.
- Anesthesia-Related Risks: The use of anesthesia carries typical risks, such as allergic reactions or respiratory issues, albeit rare.
- Bleeding and Swelling: Postoperatively, experiencing bleeding and swelling is common, but in some cases, more severe bleeding or persistent swelling may occur.
- Postoperative Infections: Infections at the surgical site can occur, necessitating antibiotic treatments and, in severe cases, graft removal.
- Graft Failure: Despite efforts, there is a risk of graft failure due to factors such as insufficient integration of the transplanted bone or complications during the healing process.
- Pressure or Pain Sensation in the Paranasal Sinuses: Some patients may experience sensations of pressure or pain in the paranasal sinuses after the lift, which may resolve over time.
- Graft Migration: The transplanted bone may migrate from its intended position, influencing the procedure’s success and requiring additional corrections.
- Donor Bone-Related Limitations: If the bone comes from another area of the patient’s body, limitations such as persistent pain or sensitivity may arise.
- Risks Associated with Dental Implants: In cases where the maxillary sinus lift is associated with dental implants, risks like implant failure or infection around the implants may occur.
Addressing these risks requires careful attention, postoperative monitoring, and, in the case of complications, timely interventions to ensure the overall success of the treatment.
Future Outlook with Galileus Cerclage Sinus®:
The future of implantology holds bright opportunities thanks to the revolutionary technique of Galileus Cerclage Sinus®. In this section, we will explore the advantages and prospects offered by this innovative procedure.
Advantages of Galileus Cerclage Sinus®:
-
- Avoids Maxillary Sinus Lifts: The primary distinction of Galileus Cerclage Sinus® is its ability to bypass traditional maxillary sinus lifts. This means patients with insufficient bone in the posterior maxillary arch can benefit from dental implants without the need for additional procedures.
- Minimizes Risks and Complications: Compared to conventional techniques, Galileus Cerclage Sinus® is designed to minimize the risks and complications associated with implantology. Its advanced surgical precision reduces the likelihood of errors and enhances the overall safety of the procedure.
- Accelerated Recovery: Thanks to its innovative design, the Galileus Cerclage Sinus® technique may allow for faster recovery compared to more invasive procedures. Patients can benefit from a quicker return to normal daily activities.
- Implant Stability and Longevity: The circumference of the maxillary sinuses with two robust dental implants, along with the anchoring of the pterygoid implant, helps ensure the stability and longevity of the implants. This is particularly crucial in posterior areas of the maxillary arch subject to greater masticatory pressures.
- Natural Aesthetics and Comfort: The Galileus Cerclage Sinus® technique not only offers a safe and functional solution but also a natural aesthetic result. The absence of artificial gum contributes to comfort and visual appearance, meeting patients’ aesthetic expectations.
Future Perspectives in Implantology with Galileus Cerclage Sinus®:
-
- Increased Adoption and Awareness: The future of implantology sees greater adoption and awareness of the Galileus Cerclage Sinus® technique. Its wider adoption could transform the landscape of implant procedures, offering a safe and innovative alternative.
- Continuous Technological Advancements: Implantology is a continuously evolving field, and Galileus Cerclage Sinus® could benefit from further technological advancements. These advancements may aim to further enhance precision, reduce intervention times, and expand its applications.
- Global Education and Adoption: Ongoing education of dental professionals on innovative techniques, including Galileus Cerclage Sinus®, will contribute to its global adoption. Sharing positive experiences and successful outcomes will increase confidence in the procedure.
In conclusion, Galileus Cerclage Sinus® offers a promising future outlook in implantology. Its ability to overcome the challenges of traditional techniques and provide a safe solution opens new horizons for patients seeking advanced implant surgery. Collaboration between surgeons and patients in exploring options like this represents a step forward toward a future of safer and more effective interventions.
Advantages of Galileus Cerclage Sinus®:
-
- Avoids Maxillary Sinus Lifts: The distinctive feature of Galileus Cerclage Sinus® is its ability to avoid traditional maxillary sinus lifts. This is crucial for patients with bone atrophy in the posterior maxillary arch, allowing for dental implants without additional procedures, simplifying the surgical path for patients.
- Minimizes Risks and Complications: The advanced surgical precision minimizes the risks and complications associated with implantology. This improved approach not only enhances the procedure’s safety but ensures reliable long-term results, contributing to overall success.
- Accelerated Recovery: The innovative design enables a quicker recovery compared to more invasive procedures. Patients benefit from a timely return to daily activities, reducing post-operative discomfort and enhancing the overall surgical experience.
- Implant Stability and Longevity: The circumferential coverage of maxillary sinuses with two robust dental implants and anchoring of the pterygoid implant contribute to ensuring stability and longevity of implants. Crucial in posterior areas subjected to greater masticatory pressures, it provides a solid foundation for fixed dental prosthetics.
- Natural Aesthetics and Comfort: In addition to providing safety and functionality, Galileus Cerclage Sinus® stands out for natural aesthetics and comfort. The absence of false gum improves visual integration, meeting patients’ aesthetic expectations and enhancing their quality of life.
In summary, avoiding maxillary sinus lifts, surgical precision, accelerated recovery, and implant stability position Galileus Cerclage Sinus® as a cutting-edge choice in implantology, offering significant benefits for patients seeking safe and effective solutions.
2. Minimizes Risks and Complications:
The Galileus Cerclage Sinus® technique stands out for its ability to minimize risks and complications associated with implant surgery. This is particularly crucial to ensure a safe and reliable experience for patients. The key points of this section are outlined below:
Advanced Surgical Precision: The advanced surgical precision of the Galileus Cerclage Sinus® technique is fundamental in minimizing errors and enhancing the effectiveness of interventions. Surgeons benefit from cutting-edge tools and methodologies, allowing them to perform procedures with unprecedented precision.
Reduction of Risks Associated with Implantology: Patient safety is an absolute priority. The Galileus Cerclage Sinus® is designed to specifically address risks commonly associated with implantology, such as infections, lacerations, or other complications. Its official approval by the European Union confirms its scientific validity and the ability to minimize such risks.
Reliable and Long-lasting Results: The reduction of risks translates into more reliable and long-lasting results for patients. The technique aims to ensure that dental implants remain stable over time, reducing the likelihood of long-term issues. This contributes to instilling confidence in patients regarding the safety and longevity of the procedure.
Accessibility to Surgeons of Varying Experience Levels: Another key aspect is the design of Galileus Cerclage Sinus® to be accessible to surgeons of varying experience levels. The intuitive approach and available training resources support the effective adoption of the technique by professionals with diverse skills, ensuring widespread dissemination.
In conclusion, the “Minimizes Risks and Complications” section emphasizes how Galileus Cerclage Sinus® distinguishes itself with a focus on safety, precision, and durability, offering an advanced solution for implant procedures.
3. Accelerated Recovery:
The Galileus Cerclage Sinus® provides a significant advantage in the post-operative recovery process, reducing healing times and allowing patients to quickly return to their normal routines. The key aspects of this section are highlighted below:
Reduced Post-operative Discomfort: The Galileus Cerclage Sinus® technique is designed with a focus on minimizing post-operative discomfort. Advanced approaches and surgical precision contribute to minimizing trauma to surrounding tissues, allowing patients to experience a significantly lower level of discomfort compared to traditional procedures.
Swelling Reduction: Accelerated recovery is further facilitated by limiting swelling associated with the procedure. Precision in implant placement and reduced trauma to soft tissues contribute to reduced swelling, enhancing patient comfort during the post-operative period.
Quick Resumption of Normal Activities: With Galileus Cerclage Sinus®, patients can quickly resume their normal daily activities. The combination of lower surgical complexity and a quicker body response to the procedure significantly shortens the post-operative rest period, improving the overall quality of the patient experience.
Optimized Post-operative Monitoring: The speed of recovery is supported by optimized post-operative monitoring protocols. Surgeons, using advanced tools, can closely track the patient’s progression and make any necessary adjustments, ensuring an efficient and obstacle-free healing process.
In conclusion, the “Accelerated Recovery” section emphasizes how Galileus Cerclage Sinus® goes beyond mere surgical effectiveness, offering patients a faster and more comfortable recovery path. This crucial element translates into an overall positive experience for those choosing this innovative implant technique.
4. Implant Stability and Longevity:
One of the distinctive features of Galileus Cerclage Sinus® is its ability to provide exceptional implant stability, ensuring long-term durability. This section explores in detail the key aspects related to this fundamental characteristic:
Precise Positioning for Maximum Stability: The Galileus Cerclage Sinus® technique stands out for its advanced surgical approach, allowing precise implant positioning. This level of precision is essential to ensure optimal stability, minimizing the risk of undesired implant movements over time.
Contact with Bone for Improved Osseointegration: The sinus-circling methodology employs robust dental implants that establish direct contact with the surrounding bone. This feature promotes better osseointegration, the process by which implants securely fuse with the jawbone. Solid osseointegration significantly contributes to the long-term stability and durability of implants.
Resistance to Chewing Forces: Galileus Cerclage Sinus® is designed to successfully address the challenges of chewing forces. The strategically anchored implants, supported by the circling structure, offer superior resistance to pressures exerted during daily chewing. This helps maintain the stability and structural integrity of the implants over time.
High-Quality Materials for Longevity: Implant longevity is also influenced by the quality of materials used. Galileus Cerclage Sinus® employs premium materials that resist wear and maintain their structural characteristics over time. This ensures the long-term durability of the implants, providing patients with a reliable and enduring implant solution.
In conclusion, the “Implant Stability and Longevity” section highlights how Galileus Cerclage Sinus® distinguishes itself by providing exceptional stability and long-term durability of implants. This feature translates into significant benefits for patients, contributing to the long-term success of the implant procedure.
5. Natural Aesthetics and Comfort:
One of the primary concerns for patients undergoing implant surgery is the aesthetics of the final result and comfort during daily use. Galileus Cerclage Sinus® is designed with particular attention to these aspects, offering a natural aesthetic experience and optimal comfort. This section explores the key details of this distinctive feature:
Customized Design for a Natural Appearance: Galileus Cerclage Sinus® employs a customized design tailored to the specific needs and anatomical characteristics of each patient. This personalized approach helps achieve a natural and harmonious appearance, blending the dental prosthesis seamlessly with the rest of the dentition. The careful design takes into account the shape, size, and color of the teeth, ensuring an aesthetic result that meets patient expectations.
High-Quality Materials for a Natural Feel: Comfort during daily use is crucial for overall patient satisfaction. Galileus Cerclage Sinus® uses high-quality materials known for their strength, durability, and, most importantly, for providing a natural feel during chewing and everyday use. Patients can enjoy a dental prosthesis that behaves similarly to natural teeth, contributing to comfort and confidence in their use.
Elimination of False Gum for Better Aesthetics: A distinctive feature of Galileus Cerclage Sinus® is the absence of a false gum, a component often present in other implant techniques. This aspect is particularly appreciated by patients, especially those who place great importance on the aesthetics of their smile. The absence of a false gum helps achieve a more natural appearance and preserves the aesthetics of the smile.
Worry-Free Experience: Galileus Cerclage Sinus® not only offers a natural appearance but also a worry-free experience for patients. The fixed dental prosthesis, supported by strategically positioned implants, provides stability that allows patients to eat, speak, and smile with confidence. This contributes to the psychological comfort of patients, enabling them to enjoy a worry-free daily life with their dental prosthesis.
In conclusion, the “Natural Aesthetics and Comfort” section emphasizes how Galileus Cerclage Sinus® stands out for its focus on smile aesthetics and patient comfort. This feature aims to ensure not only excellent clinical results but also satisfaction and confidence from patients in the appearance and functionality of their dental prosthesis.
Section 6: Risk of Failure in Traditional Procedures
Traditional procedures for maxillary sinus lifts and autologous bone grafts, although commonly used, come with a series of risks and potential complications that patients should carefully consider. In this section, we will examine the risks of failure associated with such procedures and how choosing Galileus Cerclage Sinus® can provide a safe and reliable alternative.
Post-Operative Infections: One of the primary risks in traditional procedures is posed by post-operative infections. Manipulation of bone and tissues can increase the risk of bacterial contamination, leading to infections that require additional treatments and may compromise the success of the intervention.
Insufficient Integrability of the Transplanted Bone: In cases of autologous bone grafts, there is a risk that the transplanted bone may not integrate correctly with the surrounding tissue. This can cause implant instability and potentially lead to long-term failures.
Complications Related to Autologous Bone Grafts: The use of bone tissue harvested from the patient can entail a series of complications. From difficulties in the harvesting phase to possible insufficient bone regeneration, these complications can negatively impact the final outcome.
Issues Related to Maxillary Sinus Lift: Lifting the membrane of the maxillary sinus in traditional procedures can be complex and involve risks. Tears in the membrane, if not properly managed, can lead to problems during the healing process.
Future Perspective with Galileus Cerclage Sinus®: Focusing on the future perspective, we introduce Galileus Cerclage Sinus® as an innovative and safe alternative. This revolutionary procedure eliminates the risks associated with traditional procedures, offering significant advantages such as a lower incidence of infections, better integrability of the transplanted bone, and an overall less complicated procedure.
In conclusion, understanding the risks of failure in traditional procedures underscores the importance of seeking modern and reliable alternatives like Galileus Cerclage Sinus®. The safety, stability, and lasting results offered by this innovative surgical technique make it an excellent choice for patients looking to avoid the potential drawbacks of conventional practices.
Section 7: The Benefits of Galileus Cerclage Sinus®
Galileus Cerclage Sinus® marks a revolutionary breakthrough in implantology, offering a range of significant advantages over traditional maxillary sinus lift and autologous bone graft procedures. In this section, we will delve into the detailed benefits provided by this innovative surgical technique to patients.
-
-
- Avoids Maxillary Sinus Lifts: One distinctive advantage of Galileus Cerclage Sinus® is its ability to completely avoid maxillary sinus lifts. This results in a less invasive procedure and a faster recovery, eliminating the need to lift the membrane of the maxillary sinus.
- Minimizes Risks and Complications: With Galileus Cerclage Sinus®, the risks and complications associated with traditional procedures become virtually negligible. The procedure is designed to ensure greater safety, minimizing the risk of post-operative infections, issues with bone integration, and other complications.
-
- Avoids Maxillary Sinus Lifts: One of the key advantages of Galileus Cerclage Sinus® is its ability to completely avoid maxillary sinus lifts. This means that patients can enjoy a less invasive procedure, eliminating the need to lift the membrane of the maxillary sinus. This results in a faster recovery and fewer post-operative discomforts.
-
- Minimizes Risks and Complications: The Galileus Cerclage Sinus® procedure is designed to minimize the risks and complications associated with traditional practices significantly. It reduces the risk of post-operative infections, issues with bone integration, and other unwanted outcomes. This contributes to ensuring a safer surgical experience for patients.
-
- Accelerated Recovery: Due to its less invasive nature, Galileus Cerclage Sinus® allows for an accelerated recovery compared to traditional procedures. Patients can return to their daily activities in shorter timeframes, reducing the downtime dedicated to post-operative healing.
-
- Stability and Longevity of Implants: The Galileus Cerclage Sinus® technique offers superior stability and improved longevity of implants. With two robust dental implants surrounding the maxillary sinuses, a solid anchorage is achieved, ensuring reliable and long-lasting results over time.
-
- Natural Aesthetics and Comfort: The procedure aims to preserve the natural aesthetics of the patient’s smile, ensuring that the final result is harmonious and comfortable. The absence of maxillary sinus lifts and the stability of the implants contribute to a natural feel and optimal comfort.
-
-
1. Avoids Maxillary Sinus Lifts:
The first and fundamental benefit of Galileus Cerclage Sinus® is its ability to eliminate the need for maxillary sinus lifts. This revolutionary procedure overcomes the challenge of bone atrophies in the posterior region of the maxillary arch without resorting to bone grafts or invasive procedures.
Advantages:
-
- Reduced Invasiveness: By avoiding maxillary sinus lifts, the procedure becomes less invasive, significantly reducing the impact on the treated area.
- Accelerated Recovery: Without the added complexity of sinus lifts, patients experience faster recovery and less post-operative discomfort.
- Risk Minimization: By eliminating this delicate phase, associated risks such as sinus membrane tears and potential complications are reduced.
- Shorter Procedures: The absence of maxillary sinus lifts simplifies the procedure, leading to shorter operation times and an overall more efficient experience.
- Increased Comfort: Patients benefit from greater comfort during and after the intervention, avoiding the more complex aspects of traditional procedures.
In conclusion, avoiding maxillary sinus lifts through Galileus Cerclage Sinus® not only streamlines the surgical path but also provides patients with a quicker, safer, and more comfortable solution to address the challenges of bone atrophy in the posterior region of the maxilla.
2. Minimizes Risks and Complications:
Another distinctive advantage offered by Galileus Cerclage Sinus® is its ability to minimize common risks and complications associated with traditional implantology procedures, particularly those involving maxillary sinus lifts and bone grafts.
Advantages:
-
- Patient Safety First: The procedure is designed with a primary focus on patient safety, minimizing risks and potential complications.
- Elimination of Rejection Risk: Since it does not involve autologous bone grafts, Galileus Cerclage Sinus® completely eliminates the risk of tissue rejection.
- Reduced Likelihood of Infections: The procedure lowers the likelihood of post-operative infections, thanks to its less invasive nature and the minimization of complicated processes.
- Enhanced Surgical Precision: Galileus Cerclage Sinus® employs an advanced surgical approach and cutting-edge technologies, ensuring unprecedented precision during the intervention.
- Accelerated Recovery: The reduction in risks and complications translates to a faster recovery period, allowing patients to return to their daily activities more quickly.
In summary, minimizing risks and complications through Galileus Cerclage Sinus® not only enhances the overall patient experience but also underscores a commitment to safe, efficient, and effective surgical intervention.
Section 8: Future Perspectives in Implantology with Galileus Cerclage Sinus®
Galileus Cerclage Sinus® is not just an advanced solution in the present; it promises to shape the future of implantology. Let’s explore the prospects and advancements we can expect with the widespread adoption of this revolutionary surgical technique.
-
- Dissemination and Awareness: The growing global recognition of Galileus Cerclage Sinus® is expected to continue. The dissemination of accurately communicated information through various online platforms, international conferences, and collaborations with industry professionals will contribute to increased awareness.
- Continuous Technological Advancements: With constant progress in medical technology, we anticipate further improvements in the Galileus Cerclage Sinus® procedure. The integration of cutting-edge technologies could lead to an even more precise and efficient surgical experience.
- Training and Global Adoption: Ongoing commitment to training surgeons and implantology professionals will play a key role in ensuring global adoption of Galileus Cerclage Sinus®. Specialized courses and training programs will help develop the specific skills necessary to successfully implement this innovative technique.
- Awareness Campaigns on Risks of Traditional Procedures: Targeted educational campaigns will highlight the risks associated with traditional procedures, emphasizing the importance of considering safer alternatives such as Galileus Cerclage Sinus®. Informing patients about available options will contribute to informed and conscious decision-making.
In conclusion, the future of implantology with Galileus Cerclage Sinus® looks promising, with increasing dissemination, technological advancements, and global training. Its adoption represents a milestone in improving implant surgical practice and providing patients with safe and cutting-edge solutions.
Galileus Cerclage Sinus® Procedure
The Galileus Cerclage Sinus® procedure represents an innovative surgical approach to address challenges in implantology, particularly in cases of posterior maxillary atrophy. Let’s examine in detail how the procedure is performed and how it functions.
Step 1: Patient Evaluation
Before performing Galileus Cerclage Sinus®, a comprehensive patient evaluation is essential. This assessment includes analyzing the bone structure, the size of the maxillary sinus, and the availability of bone tissue in the affected area.
Step 2: Surgical Planning
Based on the evaluation, the surgeon plans the procedure, determining the exact position of dental implants and the trajectory of sinus circling. This phase is crucial to ensure optimal precision during the surgery.
Step 3: Anesthesia and Surgical Access
Once the planning is complete, the patient undergoes anesthesia to ensure a painless intervention. Subsequently, the surgeon creates a surgical access to reach the maxillary sinus area of interest.
Step 4: Maxillary Sinus Circling
The distinctive feature of the procedure is the circling of the maxillary sinus. This involves the use of robust dental implants positioned around the maxillary sinus, ensuring stability and support. The pterygoid implant is inserted into the alveolar bone and the palatine-pterigoid basal bone, addressing posterior maxillary atrophy.
Step 5: Dental Implantation
Dental implants are then carefully inserted following the surgical plan. Precision during this phase is fundamental to ensure the correct integration of implants into the surrounding bone.
Step 6: Suturing and Post-operative Monitoring
After implant insertion, suturing is performed to close the surgical access. The patient is then closely monitored in the post-operative period to ensure proper healing and respond promptly to any complications.
How Galileus Cerclage Sinus® Works
Galileus Cerclage Sinus® stands out for its ability to avoid maxillary sinus lifts and autologous bone grafts. The sinus circling technique, along with robust dental implants, provides a stable and secure solution for patients with posterior maxillary atrophy. Its advanced surgical precision helps minimize risks and accelerates the healing process, offering long-lasting and aesthetically satisfying results.
In conclusion, Galileus Cerclage Sinus® represents a breakthrough in implantology, offering an innovative procedure that overcomes traditional challenges and paves the way for a safe and advanced solution for patients.
Galileus Cerclage Sinus® Procedure – Step 1: Patient Evaluation
The first crucial phase in the Galileus Cerclage Sinus® procedure is the comprehensive evaluation of the patient. This phase is fundamental to determine the feasibility and precision of the intervention. Let’s delve into Step 1 of the procedure in detail:
Step 1: Patient Evaluation
1.1 Patient History
The surgeon begins by gathering detailed information about the patient’s medical history, including past surgeries, and the presence of pre-existing medical conditions.
1.2 Radiographic Examination
Radiographic exams, such as computed tomography (CT) or magnetic resonance imaging (MRI), are conducted to obtain detailed images of the maxillary arch. These help assess the amount of available bone, the size of the maxillary sinus, and the surrounding anatomical structure.
1.3 Bone Structure Analysis
The surgeon carefully analyzes the bone structure of the maxillary arch, evaluating bone density and identifying any areas of atrophy or reduced bone volume.
1.4 Sizing of the Maxillary Sinus
Through the analysis of radiographic images, the size of the maxillary sinus is determined, providing crucial insights for the intervention planning.
1.5 Assessment of Patient Conditions
The overall health conditions of the patient are considered, including their healing capacity and the presence of any factors that might influence the success of the intervention.
1.6 Preliminary Planning
Based on the gathered information, the surgeon initiates preliminary planning of the intervention, identifying ideal positions for sinus circling and the placement of dental implants.
The comprehensive patient evaluation in Step 1 provides a solid foundation for the detailed planning of the Galileus Cerclage Sinus® procedure, ensuring a personalized intervention tailored to the specific needs of the patient.
Step 2: Surgical Planning
Once the patient evaluation in Step 1 is completed, Step 2 focuses on the detailed planning of the surgical intervention using the Galileus Cerclage Sinus® technique.
2.1 Definition of Circling Zones
The surgeon precisely identifies the areas of the maxillary sinus that will undergo circling. This decision is based on radiographic evaluation and the size of the maxillary sinus, ensuring a targeted and specific intervention.
2.2 Placement of Dental Implants
Based on preliminary planning, optimal positions for dental implants are determined. The accurate choice of positions contributes to the stability and integration of implants into the maxillary bone.
2.3 Calculation of Torque Force
A critical part of the planning is the calculation of the torque force required for circling the maxillary sinus. This parameter is customized for each patient, ensuring precise intervention and minimizing associated risks.
2.4 Planning of Surgical Sequence
The surgeon plans the precise sequence of intervention phases, considering the positions of circling and implants. This contributes to a smooth transition between the various stages of the operation.
2.5 Safety Considerations
Particular attention is paid to safety considerations during surgical planning, ensuring that the intervention is carried out in accordance with the highest standards for patient safety.
2.6 Discussion with the Patient
Before the intervention, the surgeon discusses the surgical planning with the patient, addresses questions, and provides necessary information to ensure the patient’s understanding and awareness.
Accurate surgical planning in Step 2 is essential to ensure a precise, safe, and efficient intervention using the Galileus Cerclage Sinus® technique.
Galileus Cerclage Sinus® Procedure: Step 9 – Definition of Cinching Zones
9.1 Identification of Critical Zones: The fourth step in the Galileus Cerclage Sinus® procedure is the definition of cinching zones. The surgeon, leveraging diagnostic images and their anatomical expertise, precisely identifies critical zones that require cinching to stabilize the implants. This phase is crucial to ensure uniform force distribution and optimal resistance in the atrophic zone of the maxillary sinus.
9.2 Surgical Marking: After identifying the critical zones, the surgeon proceeds with surgical marking. Using advanced marking techniques such as visual guidance or intraoral imaging systems, points where pterygoid and nasal implants will be positioned are accurately marked. This phase ensures the correct placement of implants, contributing to the overall stability of the implant structure.
Step 4 underscores the importance of pre-operative planning and precision in defining cinching zones. These preparatory measures are fundamental for the success of the intervention, ensuring that implants are optimally positioned to support the implant structure in the long term.
Galileus Cerclage Sinus® Procedure: Step 10 – Surgical Sequence Planning
10.1 Personalized Surgical Sequence: The fifth step in the Galileus Cerclage Sinus® procedure is the detailed planning of the surgical sequence. Each patient is unique, and the surgical sequence is customized based on specific anatomical conditions and individual needs. This customization allows the surgeon to tailor the procedure to the unique characteristics of the patient, maximizing the effectiveness of the intervention.
10.2 Optimization of Operative Times: During this phase, the surgeon optimizes operative times to minimize inconvenience for the patient. Accurate planning enables the procedure to be performed efficiently while ensuring maximum precision. The surgical sequence is designed to address specific challenges of the Galileus Cerclage Sinus® procedure in a targeted manner.
Step 11 emphasizes the tailored approach of this surgical technique, highlighting how accurate planning and customization of the surgical sequence contribute to the overall success of the intervention.
Galileus Cerclage Sinus® Procedure: Step 11 – Safety Considerations
11.1 Patient Safety as Top Priority: The sixth step in the Galileus Cerclage Sinus® procedure involves safety considerations, with the absolute priority being the health and safety of the patient. During this phase, the surgeon ensures that all necessary measures are taken to provide a safe and controlled surgical environment.
11.2 Continuous Monitoring: Continuous monitoring systems are implemented to constantly assess the patient’s vital parameters during the intervention. This real-time monitoring allows the surgical team to respond promptly to any variations and maintain a safe surgical environment.
11.3 Standard Safety Procedures: During Step 6, all standard surgical safety procedures are rigorously followed. This includes the thorough sterilization of instruments, the use of protective attire, and the adoption of practices that minimize the risk of infections or post-operative complications.
Step 6 emphasizes the commitment to patient safety, ensuring that every precaution is taken to provide a safe and protected surgical environment.
Galileus Cerclage Sinus® Procedure: Step 12 – Anesthesia and Surgical Access
Anesthesia: The third step in the Galileus Cerclage Sinus® procedure begins with administering anesthesia to the patient. This step is crucial to ensure the patient’s comfort during the surgical intervention. Anesthesia is administered following standard practices for dental surgical procedures, ensuring that the patient experiences no pain or discomfort throughout the entire procedure.
Surgical Access: Once the anesthesia has taken effect, the surgeon proceeds with surgical access. This involves creating targeted incisions to gain adequate access to the working area. In the Galileus Cerclage Sinus® technique, surgical access is precisely planned to allow optimal positioning of pterygoid and nasal implants.
During this step, the surgeon leverages their experience and anatomical knowledge to ensure safe and precise access to the maxillary sinus area. Attention is focused on minimizing trauma to surrounding tissues and optimizing conditions for the subsequent placement of implants.
Step 3 of the Galileus Cerclage Sinus® establishes the foundation for the success of the intervention, ensuring that the patient is adequately anesthetized, and surgical access is performed with the utmost accuracy and care.
Placement of Implants in Galileus Cerclage Sinus® Technique
In the context of the Galileus Cerclage Sinus® technique, precise implant placement plays a crucial role in maximizing stability and promoting optimal healing. Let’s examine in detail where pterygoid and nasal implants are inserted.
1. Pterygoid Implants (18/28): Pterygoid implants are strategically placed in the posterior molars, typically in the 18/28 area. Their position aims to provide fundamental structural support in the maxillary sinus region. The goal is to ensure even distribution of masticatory forces, contributing to the overall stability of the entire implant structure.
2. Nasal Implants (15/25): Nasal implants play a key role in closing the cerclage around the maxillary sinus. Positioned towards the nasal spine in the 15/25 area, these implants contribute to creating a second pillar of resistance around the atrophic zone of the maxillary sinus. This targeted arrangement promotes structural solidity and long-term durability of the implants, ensuring a safe and reliable implant solution for the patient.
The accurate placement of pterygoid and nasal implants is an integral part of the Galileus Cerclage Sinus® methodology, aiming to overcome challenges related to posterior maxillary atrophy and provide patients with an advanced and long-lasting implant solution.
Galileus Cerclage Sinus® Procedure: Step 13 – Patient Discussion
13.1 Clear Communication: The seventh step in the Galileus Cerclage Sinus® procedure focuses on clear communication with the patient. The surgeon discusses the procedure details, answers questions, and provides all necessary information to ensure the patient’s awareness and understanding.
13.2 Confirmation of Informed Consent: During this phase, the patient confirms informed consent, demonstrating a full understanding of the procedure, associated risks, and potential benefits. Open and transparent communication is crucial to instill confidence in the patient and ensure an informed decision.
13.3 Expectation Management: The surgeon manages the patient’s expectations, offering realistic information about the procedure, recovery times, and expected outcomes. This phase is essential for establishing a trusting relationship between the patient and the surgical team.
Step 14 emphasizes the importance of effective communication and patient involvement in the decision-making process. Clear understanding and patient awareness are crucial for the success of the procedure and their healing journey.
Section 14: The Future of Implantology – Choosing the Best Today
14.1 Stay Informed about Available Options:
The constant evolution in implantology provides new perspectives for the future of oral surgery. In this section, we will explore the importance of making informed decisions and choosing cutting-edge technologies to ensure superior and lasting results.
14.2 Galileus Cerclage Sinus®: The Future of Implant Surgery:
Choosing Galileus Cerclage Sinus® means embracing the future of implant surgery. This revolutionary technique eliminates the need for sinus lifts and autologous bone grafts, offering a safe, effective, and aesthetically satisfying approach.
14.3 Long-lasting Benefits:
Opting for Galileus Cerclage Sinus® means enjoying lasting benefits. Well-positioned implants, supported by this technique, provide stability, strength, and long-term durability, minimizing the risks associated with conventional procedures.
14.4 Invest in Your Oral Health:
Oral health is a long-term investment. Choosing Galileus Cerclage Sinus® is a step towards a safe and durable implant solution. This decision positively impacts the quality of life, providing a solid foundation for a healthy and functional mouth.
14.5 Choosing the Best Today for a Lasting Smile:
In conclusion, the future of implantology is in the hands of those making informed decisions today. Galileus Cerclage Sinus® emerges as the best choice, redefining the standards of implant surgery and paving the way for excellent and lasting results.
Choosing Galileus Cerclage Sinus® means embracing the forefront of implant surgery and ensuring a radiant smile for the future. Staying informed, making conscious choices, and opting for excellence are fundamental steps for optimal oral health.
15.1 Stay Informed about Available Options
In a constantly evolving world, implant surgery also experiences ongoing progress and innovations. Being informed about the various available options is crucial for making conscious decisions about one’s oral health. In recent years, research and development in implantology have led to the creation of cutting-edge solutions, such as Galileus Cerclage Sinus®.
Importance of Awareness
Understanding implant treatment options is vital for patients seeking to address challenges related to bone deficiency in the posterior region of the maxilla. Being informed about the latest technologies and methodologies allows for making educated decisions, considering differences between conventional techniques and revolutionary alternatives like Galileus Cerclage Sinus®.
Access to Informative Resources
Awareness of available options can be gained through various sources, including reliable websites, scientific publications, and consultations with implantology professionals. Accessing trustworthy informative resources provides a clear overview of the latest technologies and treatments in the field.
Patient’s Role in Exploring Options
Patients play an active role in the decision-making process regarding their oral health. Exploring available options, understanding techniques, and evaluating the benefits and risks of each solution contribute to an informed and personalized choice.
Collaboration with Implantology Professional
Open and collaborative dialogue with the implantology professional is crucial for an informed choice. Asking questions, discussing concerns, and exploring options together with the professional allows for a thorough understanding of the alternatives available.
In conclusion, being informed about available options is the first step towards a conscious decision in choosing implant solutions. In the next segment, we will explore the revolutionary role of Galileus Cerclage Sinus® in the future of implant surgery.
15.2 Lasting Benefits
Galileus Cerclage Sinus® offers lasting benefits that go beyond simply addressing challenges related to bone deficiency in the posterior region of the maxilla. This section will explore in detail the long-term benefits that make this technique an innovative and enduring choice in the field of implantology.
-
- Continuous Implant StabilityOne distinctive feature of Galileus Cerclage Sinus® is its ability to ensure continuous stability of implants over time. Thanks to its advanced design and innovative surgical methodology, this technique provides a solid foundation for dental implants, helping to prevent instability issues in the long run.
- Minimization of Failure RiskMinimizing the risk of failure is another lasting advantage of Galileus Cerclage Sinus®. By eliminating the need for maxillary sinus lifts and minimizing risks associated with traditional procedures, this technique offers a reliable solution that translates into successful long-term results.
- Reduction of Overall Healing PeriodThe prospect of quicker and less invasive healing is a benefit that reflects in the long term. By reducing the overall healing period, Galileus Cerclage Sinus® allows patients to quickly enjoy the benefits of a new dental structure without enduring lengthy recovery phases.
- Improved Quality of LifeThe positive effects of Galileus Cerclage Sinus® extend beyond purely dental aspects. The quality of life for patients improves due to implant stability, reduced risks of complications, and effective restoration of masticatory and speech functions.
- Reduced Long-Term CostsThe durability and reliability of Galileus Cerclage Sinus® translate into reduced long-term costs for patients. Minimizing the risks of failure and the need for additional procedures contributes to more efficient financial management over the years.
In conclusion, the lasting benefits of Galileus Cerclage Sinus® position it as a long-term choice for those seeking a safe and effective implant solution. In the next section, we will explore the future prospects of this revolutionary technique and its potential impact on the evolution of implantology.
15.3 Investing in Your Oral Health
Investing in one’s oral health is a decision that can lead to significant benefits for overall well-being. In this section, we will explore how choosing Galileus Cerclage Sinus® represents a valuable investment in long-term oral health.
-
- Prevention of Future IssuesThe Galileus Cerclage Sinus® technique stands out for its ability to prevent future problems associated with bone deficiency in the posterior region of the maxilla. Avoiding maxillary sinus lifts and autologous bone grafts significantly reduces the likelihood of long-term complications, providing a solid foundation for sustainable oral health.
- Minimization of RisksInvesting in one’s oral health with Galileus Cerclage Sinus® means minimizing the risks associated with traditional procedures. The reduction of failure risk, complications, and prolonged healing periods contributes to an overall safer and less stressful experience for the patient.
- Improved Quality of LifeOptimal oral health directly contributes to overall quality of life. Galileus Cerclage Sinus®, by offering a stable and lasting solution, allows patients to fully enjoy daily activities, from worry-free meals to unimpeded communication.
- General Well-beingOral health is closely linked to general well-being. Investing in Galileus Cerclage Sinus® not only preserves the health of teeth and gums but can also positively impact other aspects of health, such as digestion and posture.
- Economic SustainabilityWhile it may seem like an initial investment, choosing Galileus Cerclage Sinus® translates into long-term economic sustainability. The reduction of costs associated with potential complications and additional procedures contributes to more efficient financial management over time.
In conclusion, investing in your oral health through Galileus Cerclage Sinus® is a significant step toward a worry-free future for dental health. The next section will explore the future prospects of this technique and how it may shape the evolution of implantology.
If you are a patient facing severe posterior maxillary bone loss and are unsure where to turn, you are in the right place: the portal for solutions to your dental problems. Despite your bone deficiency and reluctance to undergo both bone grafts and significant maxillary sinus lifts, and even if you have minimal interest in procedures involving quad zygomatic implants, feel free to send us a message on WhatsApp at +393887527525. We will respond within 24 hours to definitively address your issues with the best surgical technique available today for addressing upper maxillary atrophy.
We are here to help you overcome your challenges related to upper maxillary atrophy. If you are seeking the best solution without opting for bone grafts or extensive maxillary sinus lifts, and if you wish to avoid procedures involving quad zygomatic implants, we are ready to offer you the best surgical technique available today.
Feel free to send us a message on WhatsApp at +393887527525, and we will respond within 24 hours to discuss your needs and find the optimal solution for you. With our extensive experience in implant surgery and the use of the Galileus Cerclage Sinus® technique, we guarantee excellent results with the utmost in masticatory function, aesthetics, and comfort.
Do not hesitate to contact us to definitively address your dental issues. We are here to provide you with the highest level of care using the most advanced and personalized technology.